The SARS-CoV-2 virus that caused the COVID-19 pandemic is a novel coronavirus that has never caused infections in humans before. Thanks to the achievements in molecular biology, the structure of this virus was rapidly determined, and a method for its detection in the human body was developed. Identifying infected persons allows isolating them, which helps to stop the spread of the virus much more effectively. A professor of the Institute of Biomedical Sciences of the Faculty of Medicine at Vilnius University (VU MF), immunologist, Dr. Dainius Characiejus explains about SARS-CoV-2 virus attacks and immune defense of human body.
Immunity Is a Weapon Against the Virus
"It goes without saying that quarantine alone will not eradicate the virus. It will survive and, given the opportunity, will penetrate our society again. We will only be able to be free of the virus, if we are immune to it," the professor says. Recently, vaccines have been widely discussed in the media as a possible means of protection against the virus. However, while waiting for the vaccine, we need to remember that our immune system fights viruses too.
Like most infectious agents, the SARS-CoV-2 virus does not cause the disease in all people who come into contact with a diseased person. Most people experience light or even no symptoms, while for some people the disease is fatal. Although the SARS-CoV-2 virus has not yet been sufficiently studied, it can be argued that the virus is particularly unpredictable in terms of infection and disease progression.
According to Dr. Dainius Characiejus, if we understood why some people do not contract the disease or experience only its mild form after a contact with a sick person, we might know how to prevent SARS-CoV-2 infection, its severe complications, and death.
Our body’s first barrier of protection against viruses, the so-called innate immune response, is ready to protect us from birth. Interferons and cells called "natural killers" constantly protect our bodies from viruses. These are signaling molecules that are produced by the immune system cells. These cells are infected with a virus, thus transmitting the alarm signal to other cells, so that they can produce enzymes which inhibit virus multiplication. According to the professor, there is evidence that interferon production in the elderly is reduced, which could partially explain the poorer prognosis of SARS-CoV-2 virus infection among the elderly.
 Prof., Dr. Dainius Characiejus
Prof., Dr. Dainius Characiejus
Innate Immunity Is Weaker Than Acquired
Research has shown that viruses can only multiply inside cells. When this happens, there is nothing left but to destroy the virus-infected cell. This is what natural killer cells do, but the innate immune response is not very strong. On the other hand, long-term and effective protection against infectious agents may be provided by the acquired immune response which is governed by the "adaptive immune system".
The so-called "adaptive immune system" helps us to adapt and live in an environment with constant risk of infections. The weapons of this system are antibodies and another type of killer cells – cytotoxic T lymphocytes. Antibody molecules encapsulate the virus that has entered the body, and it can no longer penetrate other cells. Cytotoxic T lymphocytes destroy virus-infected cells.
The adaptive immune system has a highly targeted action against the infectious agent. In addition, this part of the immune system exhibits memory, i.e., next time the virus enters the body, the response is much quicker and stronger. However, for the adaptive immune system to start working, certain preparations need to be made, such as the production of specific antibodies and cytotoxic T lymphocytes. This process usually takes up to a few weeks.
“In layman’s terms it can be explained that two locks need to be opened to trigger the adaptive immune system. Each "lock" is a certain signal that the cells of the immune system must transmit to each other," Dr. Dainius Characiejus says.
Immunity Sends a Signal
The first signal from antigen-presenting cells is received by T lymphocytes with their antigen receptor. Antigen-presenting cells are dendritic cells and macrophages that have the ability to distinguish between short-term and long-term hazards. The carrier of short-term hazard is simply destroyed, but if the antigen-presenting cells sense that the infectious agent may be dangerous for a long time, the signal is transmitted to T lymphocytes.
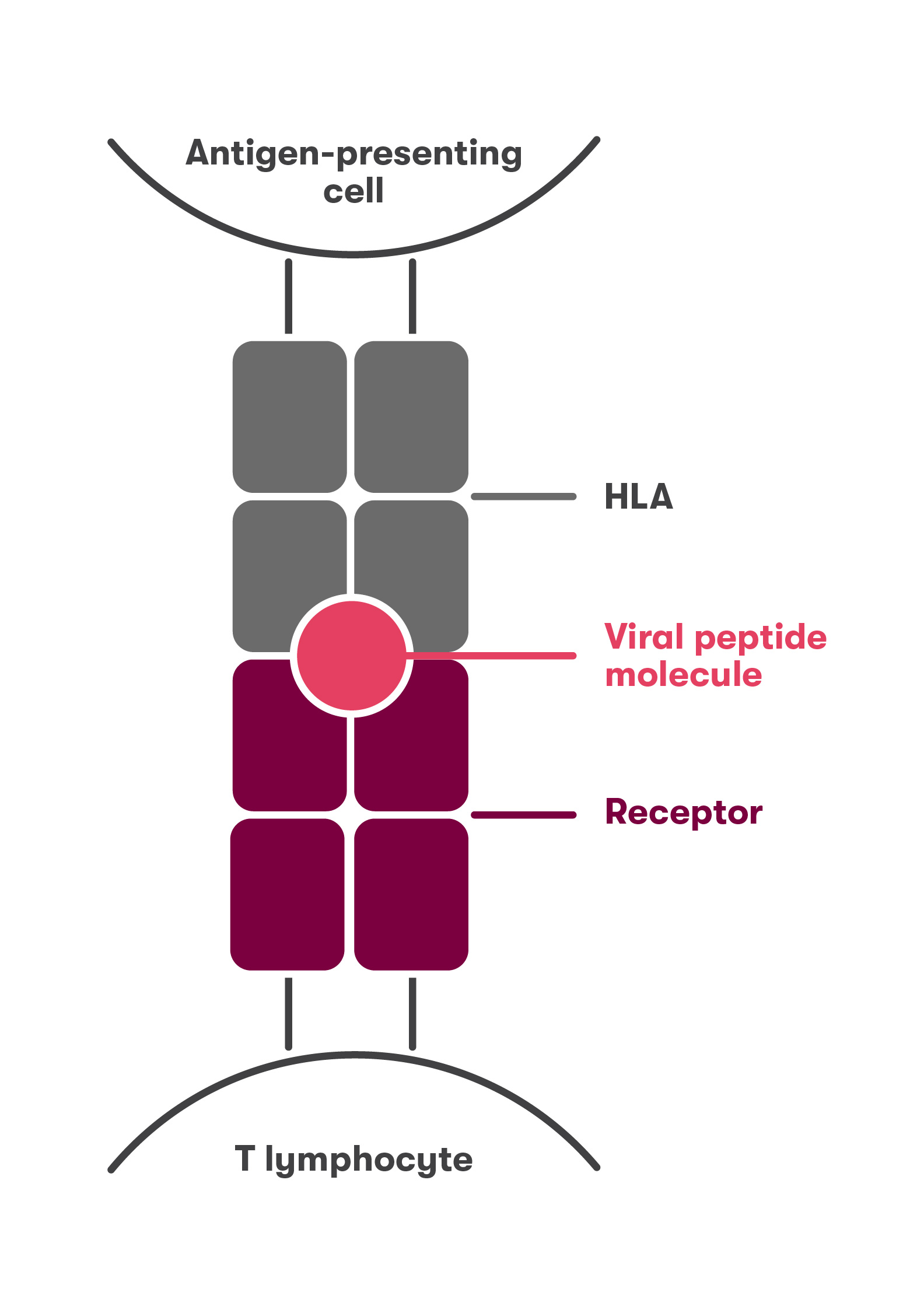
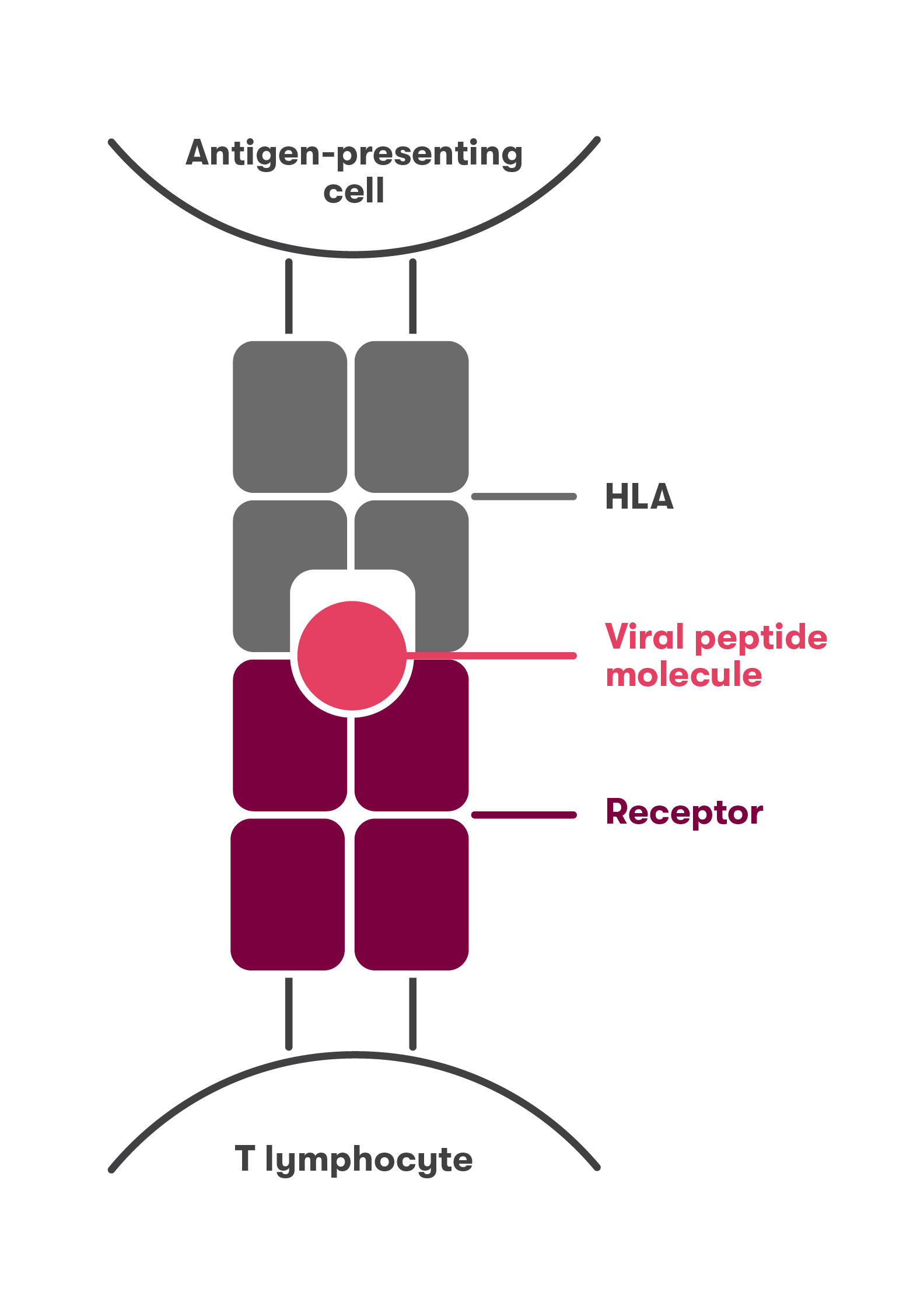
According to the researcher, during SARS-CoV-2 infection this signal may be a viral peptide. T lymphocytes cannot recognize a foreign peptide if it is not on the cell surface and not bound to a so-called HLA molecule. The genes encoding HLA molecules are highly polymorphic – it means that each of us has different HLA molecules. These molecules can bind many different peptides, but not all possible ones, and the activation of the adaptive immune system depends on the strength of that binding.
Resistance to a variety of infections, including tuberculosis, smallpox, HIV, hepatitis B, and influenza, has been found to be associated with certain types of HLA molecules. If the viral peptide molecule, the HLA molecule, and the T lymphocyte receptor bind very strongly (Fig. 1), then the adaptive immune system is strongly activated and the infection can be controlled before it can occur. If the binding between the viral peptide molecule, the HLA molecule, and the T lymphocyte receptor is weak (Fig. 2), then the adaptive immune system is not activated and the viral infection spreads.
Immune System Can "Shoot Itself in the Foot"
Severe disease develops in about 15% of people infected with the SARS-CoV-2 virus. A so-called cytokine storm begins, when the cells of the immune system over-activate each other and stimulate inflammation. Uncontrolled inflammation irreversibly damages the lungs, causes blood clots to form in the blood vessels. This way, the immune system "shoots itself in the foot" while trying to protect the patient's body. According to Dr. Dainius Characiejus, there are some prospective treatments which aim to stop the cytokine storm by using medications to block some of them, such as interleukin-6.
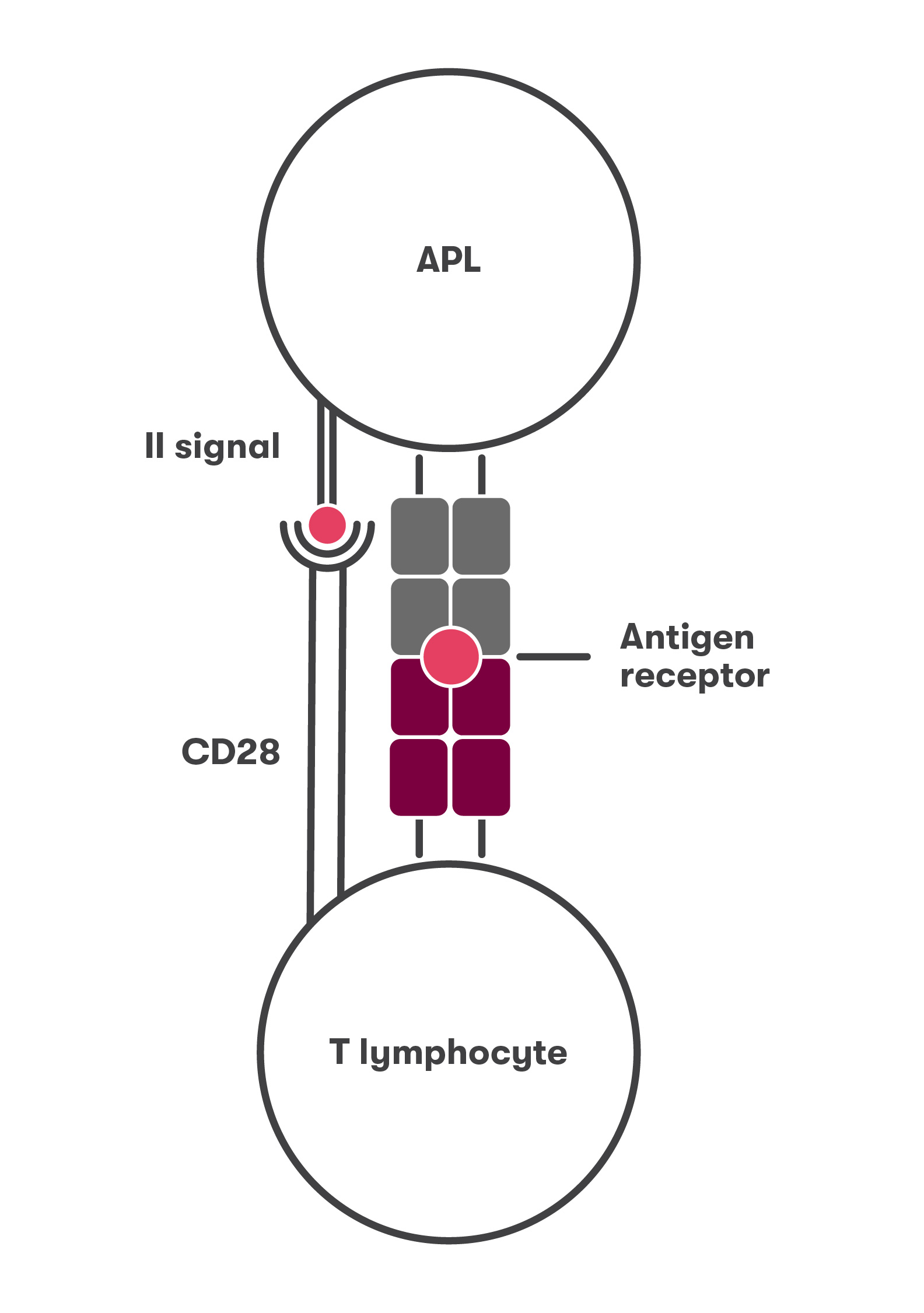
Most commonly, these cytokine storms occur in people over 65 years of age. This is due to the second lock that launches the adaptive immune system – the second signal that T lymphocytes must receive. The signal is received by T lymphocyte CD28 receptors (Fig. 3). According to the researcher, as the body and immune system age, T lymphocytes lose this receptor (Fig. 4), resulting in a decrease of up to 40% and even less at old age, while almost all children’s lymphocytes have CD28 receptors.
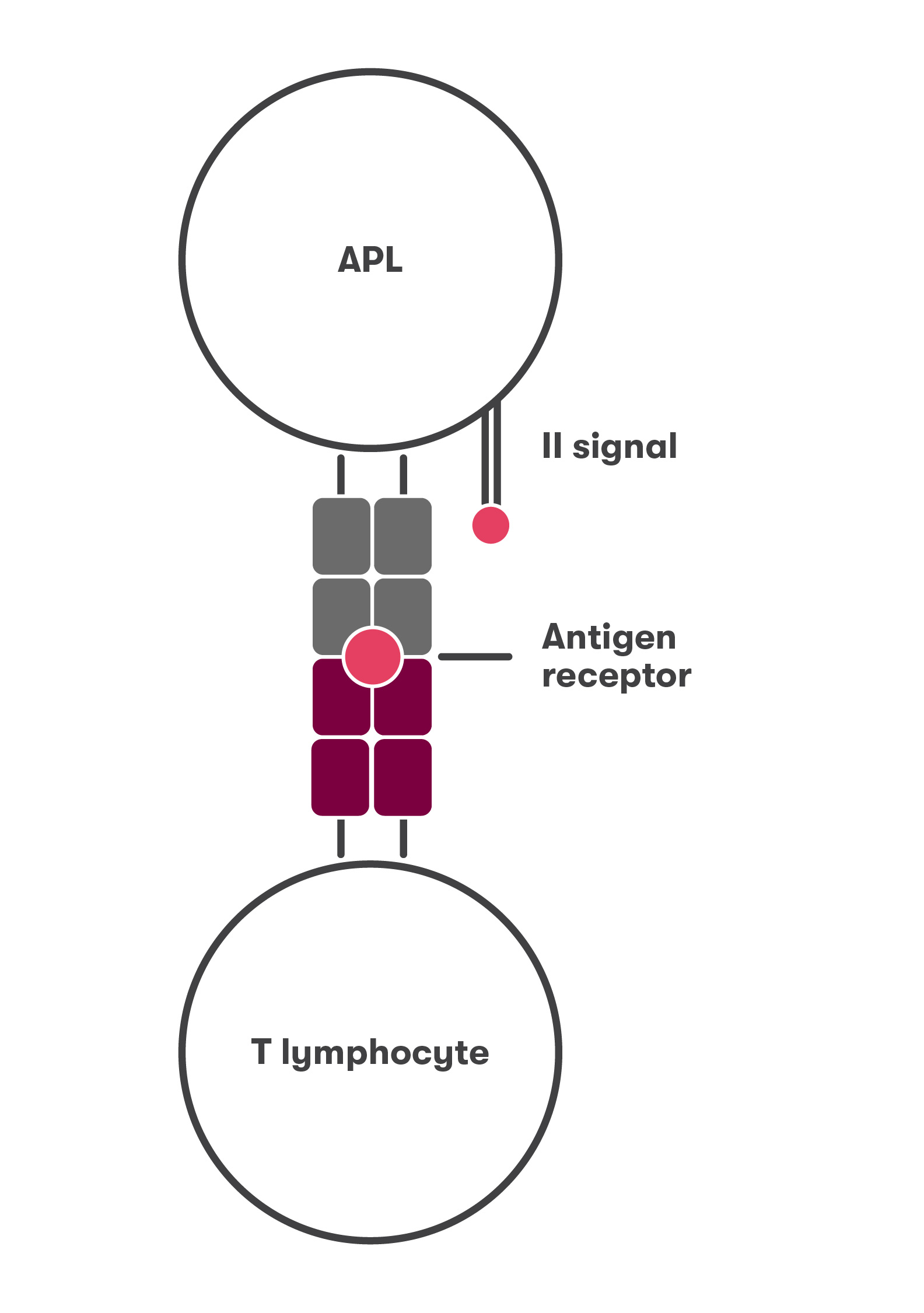
"Unfortunately, these lymphocytes can only be studied in the human body, so we have very little knowledge about them," the scientist admits. In bodies of lab mice, lymphocytes do not lose the CD28 molecule, possibly due to the fact that mice live significantly shorter than humans. However, the scarce data in the literature allows to form a certain picture of aged T lymphocytes without CD28 receptor.
"It turns out that these lymphocytes have lost the ability to accurately identify a new infectious agent, but can produce cytokine storm-causing substances without choosing to kill the body’s cells. What role do these lymphocytes play in patients with COVID-19 infection? Without research, it is not possible to answer this question yet," Dr. Dainius Characiejus says.
